Charles Corfield continues his weekly COVID-19 update with a look at an unexpected way of gathering research through digital thermometers and he wonders if a simplistic approach might be a way to ward off the virus. Please check back on Monday’s for additional updates from Charles.
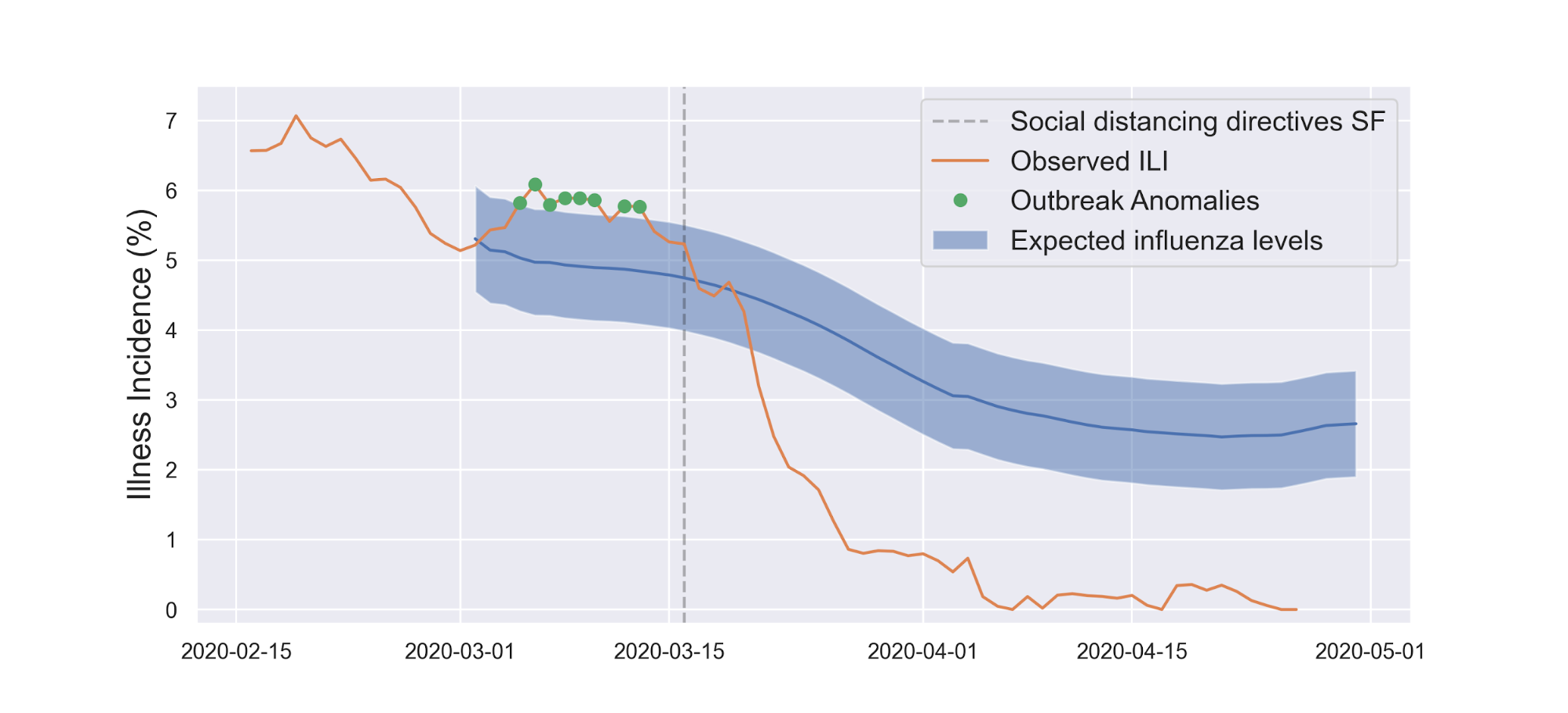
From the Kinsa data, not only did social distancing work against COVID-19, it also limited the spread of other illnesses (which have fevers). The abbreviation "ILI" in their graph stands for "Influenza-Like Illness".
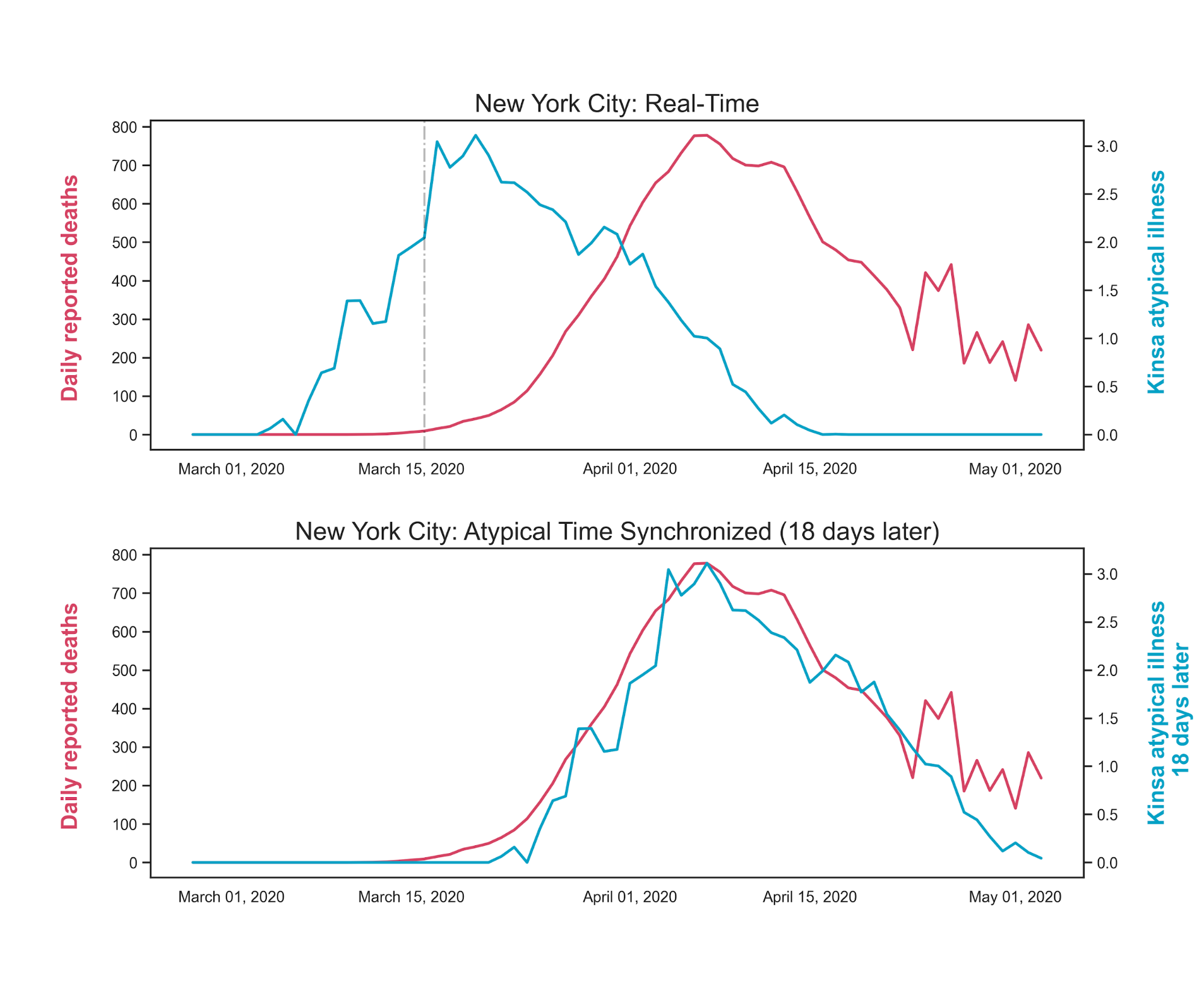
Another epidemiological guesstimate which the Kinsa statisticians have shored up is the time from onset of illness to death, or "TTM" (time to mortality). The onset of symptoms is when someone is likely to reach for the thermometer to see if they are running a fever. Lots of people did this in New York City, and you can see a very clear correlation between the curves for anomalous fevers and deaths. In my earlier e-mails I used a guess of a few weeks for TTM, Kinsa folks have nailed it to 18 days from onset of symptoms:
The Kinsa folks are to be commended on demonstrating such a simple and elegant means to produce valuable epidemiology insights with anonymized data.
On other fronts, researchers continue to be busy setting new records in the timeliness of communicating their findings. Last week I mentioned the history of the four corona viruses (HCoV's) which are responsible for 20-30% of common colds. Is it possible that exposure to one of these other viruses confers partial immunity to sars-cov-19? A team at the NHS looked for evidence of cross-reactivity of antibodies to common cold HCoV's and Sars-CoV-2 and found evidence in favor. This is still in the preliminary bucket but may be part of the explanation regarding the range of susceptibility we have seen, and why most people don't seem to be bothered by Sars-CoV-2.
In an earlier blog, my hunch was that we should be thinking about COVID-19 from the perspective of sepsis. Researchers at Stanford have now compared the cytokine signaling in patients who are currently hospitalized for COVID-19 with blood samples drawn from pre-pandemic patients with sepsis. In a nutshell: there is no difference between the two groups. I think this strengthens the case that while the virus is the root cause, the thing which hospitalizes and kills patients is a loss of regulatory control over inflammatory signaling pathways.
Two important clues are (a) the observation that smoking appears to be protective; (b) the reports of loss of smell/taste. While the primary purpose of the virus's spike protein may be to stick to ACE2 receptors in order to break in to a host cell, components of the spike probably stick to other things as well, and I expect that researchers will discover that if they create cell cultures which express receptors for 5HT3 and α7nACh they will find that the virus adheres to these, too. These are receptors implicated in taste/smell and in the regulation of inflammation. In the latter case, it is as though the virus puts a rock under the inflammatory brake pedal. Once the inflammatory response to the virus is well under way, the body is unable to restrain it. The nicotine, which smokers get from cigarettes, tends to keep the brake pedal somewhat depressed in the first place, which is why they are less likely to go to hospital. On the other hand, for overweight/obese/diabetic folks their foot is already pushing on the inflammatory gas pedal, and so they are more likely to end up in hospital. It may turn out that, once someone is hospitalized, you need to give them something to dislodge the rock under the brake pedal.
I anticipate that we will start to see clinical trials registered for potential "rock-removers" in the near future. The sepsis perspective also explains why things which don't work for sepsis, don't work for severe COVID-19 either (e.g. steroids), but compounds which inhibit blood clotting seem to help some patients (note that clotting is a feature of sepsis). While it is our nature to find complicated, whiz-bang solutions to problems, the minimalist in me wonders if there is also a low-tech approach: any takers for putting a bottle of aspirin and pack of nicotine gum in the medicine cabinet?
[Charles standard disclaimer is that none of the foregoing constitutes medical advice, etc.]